Archive for June, 2020
LOCKDOWN LUNACY: The Thinking Person’s Guide

Great article from the brilliant JB Handley and Children’s Health Defense.
By J.B. Handley, CHD Contributing Writer
For anyone willing to look, there are so many facts that tell the true story, and it goes something like this:
Knowing what we know today about COVID-19’s Infection Fatality Rate, asymmetric impact by age and medical condition, non-transmissibility by asymptomatic people and in outdoor settings, near-zero fatality rate for children, and the basic understanding of viruses through Farr’s law, locking down society was a bone-headed policy decision so devastating to society that historians may judge it as the all-time worst decision ever made. Worse, as these clear facts have become available, many policy-makers haven’t shifted their positions, despite the fact that every hour under any stage of lockdown has a domino-effect of devastation to society. Meanwhile, the media—with a few notable exceptions—is oddly silent on all the good news. Luckily, an unexpected group of heroes across the political landscape—many of them doctors and scientists—have emerged to tell the truth, despite facing extreme criticism and censorship from an angry mob desperate to continue fighting an imaginary war.
My goal is to engage in known facts. You, the reader, can decide if all of these facts, when you put them together, equate to the story above.
Fact #1: The Infection Fatality Rate for COVID-19 is somewhere between 0.07-0.20%, in line with seasonal flu
The Infection Fatality Rate math of ANY new virus ALWAYS declines over time as more data becomes available, as any virologist could tell you. In the early days of COVID-19 where we only had data from China, there was a fear that the IFR could be as high as 3.4%, which would indeed be cataclysmic. On April 17th, the first study was published from Stanford researchers that should have ended all lockdowns immediately, as the scientists reported that their research “implies that the infection is much more widespread than indicated by the number of confirmed cases” and pegged the IFR between 0.12-0.2%. The researchers also speculated that the final IFR, as more data emerged, would likely “be lower.” For context, seasonal flu has an IFR of 0.1%. Smallpox? 30%.
As the first study to peg the IFR, the Stanford study came under withering criticism, prompting the lead researcher, Dr. John Ioannidis to note,
“There’s some sort of mob mentality here operating that they just insist that this has to be the end of the world, and it has to be that the sky is falling. It’s attacking studies with data based on speculation and science fiction. But dismissing real data in favor of mathematical speculation is mind-boggling.”
Like all good science, the Stanford data on IFR has now been replicated so many times that our own Centers for Disease Control came out this week to announce that their ‘best estimate’ showed an IFR below 0.3%. In this article on the CDC’s new data, they also highlighted how the cascading declines in IFR has removed all the fears of doomsday:
That “best estimate” scenario also assumes that 35 percent of infections are asymptomatic, meaning the total number of infections is more than 50 percent larger than the number of symptomatic cases. It therefore implies that the IFR is between 0.2 percent and 0.3 percent. By contrast, the projections that the CDC made in March, which predicted that as many as 1.7 million Americans could die from COVID-19 without intervention, assumed an IFR of 0.8 percent. Around the same time, researchers at Imperial College produced a worst-case scenario in which 2.2 million Americans died, based on an IFR of 0.9 percent.
If you’re still unconvinced that the IFR of COVID-19 is roughly in line with a bad flu season, the most comprehensive analysis I have seen comes from Oxford University, who recently stated:
“Taking account of historical experience, trends in the data, increased number of infections in the population at largest, and potential impact of misclassification of deaths gives a presumed estimate for the COVID-19 IFR somewhere between 0.1% and 0.41%.”
Finally, just last week, Stanford’s Dr. Ioannidis published a meta-analysis (because so many IFR studies have been done around the world in April and early May) where he analyzed TWELVE separate IFR studies and his conclusion is so good, I’ll just leave you with it:
The infection fatality rate (IFR), the probability of dying for a person who is infected, is one of the most critical and most contested features of the coronavirus disease 2019 (COVID-19) pandemic. The expected total mortality burden of COVID-19 is directly related to the IFR. Moreover, justification for various non-pharmacological public health interventions depends crucially on the IFR. Some aggressive interventions that potentially induce also more pronounced collateral harms1 may be considered appropriate, if IFR is high. Conversely, the same measures may fall short of acceptable risk-benefit thresholds, if the IFR is low…Interestingly, despite their differences in design, execution, and analysis, most studies provide IFR point estimates that are within a relatively narrow range. Seven of the 12 inferred IFRs are in the range 0.07 to 0.20 (corrected IFR of 0.06 to 0.16) which are similar to IFR values of seasonal influenza. Three values are modestly higher (corrected IFR of 0.25-0.40 in Gangelt, Geneva, and Wuhan) and two are modestly lower than this range (corrected IFR of 0.02-0.03 in Kobe and Oise).
Opinion #1: Dr. Scott Atlas
Soon after the Stanford study released its data (he wasn’t a study author), Stanford’s Dr. Scott Atlas published an opinion piece in The Hill newspaper with the title, “The data is in — stop the panic and end the total isolation.” He wrote:
The recent Stanford University antibody study now estimates that the fatality rate if infected is likely 0.1 to 0.2 percent, a risk far lower than previous World Health Organization estimates that were 20 to 30 times higher and that motivated isolation policies…Let’s stop underemphasizing empirical evidence while instead doubling down on hypothetical models. Facts matter.
Facts do matter, but no one listened. Dr. Atlas’ article also helps frame Fact #2.
Fact #2: The risk of dying from COVID-19 is much higher than the average IFR for older people and those with co-morbidities, and much lower than the average IFR for younger healthy people, and nearing zero for children
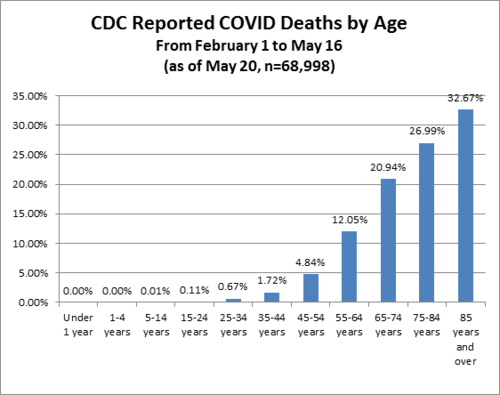
In January 2020, Los Angeles had an influenza outbreak that was killing children, the LA Times noted that “an unlikely strain of influenza has sickened and killed an unusually high number of young people in California this flu season.” COVID-19 is the opposite of that. Stanford’s Dr. Ioannidis said, “Compared to almost any other cause of disease that I can think of, it’s really sparing young people.”
Italy reported three days ago that 96% of Italians who died from COVID-19 had “other illnesses” and were, on average, 80 years old. From Bloomberg:
“The latest numbers show that new cases and fatalities have a common profile: mostly elderly people with previous illnesses,” ISS chief Silvio Brusaferro said at a news conference Friday.
The best age stratification data I have seen comes from Worldometers.info. Here’s their chart estimating death rate by age group. Please note that death rate is MUCH higher than IFR because death rate uses confirmed COVID-19 cases as the denominator, but it shows you how different the fatality rates are by age:
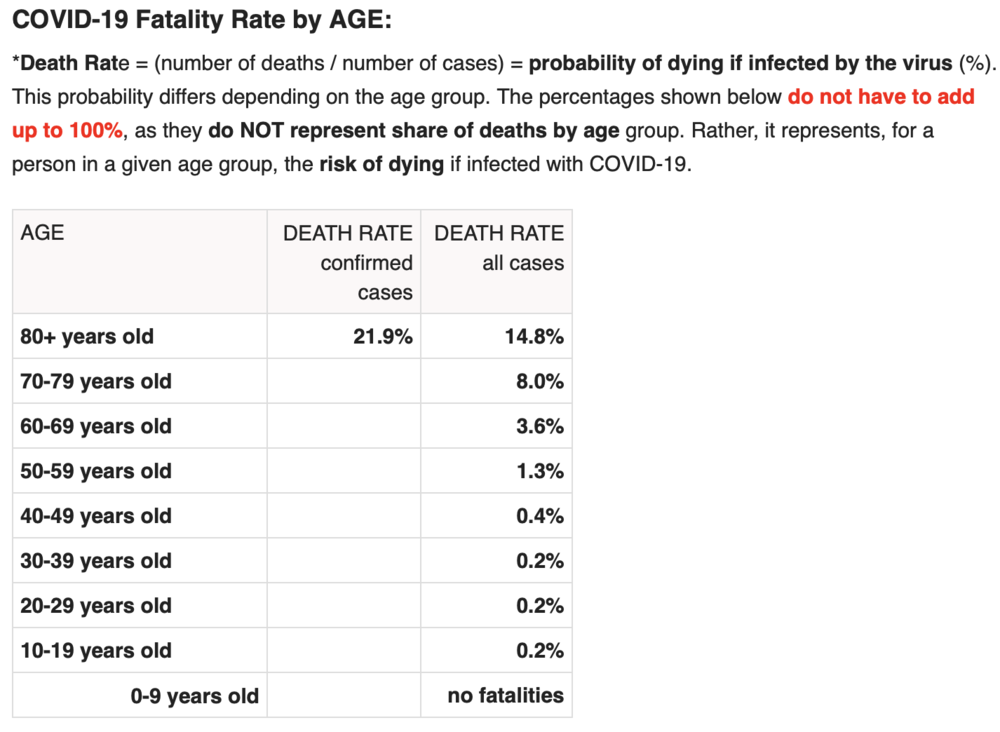
While this data is “crude”, it’s safe to extrapolate that an 80+ year-old person has a serious risk of dying from COVID-19 while a child faces almost no risk. This fact should drive policy, as Dr. Atlas explains:
Of all fatal cases in New York state, two-thirds were in patients over 70 years of age; more than 95 percent were over 50 years of age; and about 90 percent of all fatal cases had an underlying illness. Of 6,570 confirmed COVID-19 deaths fully investigated for underlying conditions to date, 6,520, or 99.2 percent, had an underlying illness. If you do not already have an underlying chronic condition, your chances of dying are small, regardless of age. And young adults and children in normal health have almost no risk of any serious illness from COVID-19.
Consider this excellent article from the British Medical Journal, titled “Shielding from covid-19 should be stratified by risk” written by Cambridge University professors:
Protecting those at most risk of dying from covid-19 while relaxing the strictures on others provides a way forward in the SARS-CoV-2 epidemic, given the virus is unlikely to disappear in the foreseeable future. Such targeted approaches would, however, require a shift away from the notion that we are all seriously threatened by the disease, which has led to levels of personal fear being strikingly mismatched to objective risk of death. Instead, the aim should be to communicate realistic levels of risk as they apply to different groups, not to reassure or frighten but to allow informed personal decisions in a setting of necessary uncertainty.
As one simple example: closing schools makes almost no sense given what we know about COVID-19, while protecting teachers over the age of 60—to pick a somewhat defensible age boundary—may well make sense. This is why so many countries who seem to respect data more than we do here in the U.S. have already re-opened their schools. In fact, Denmark’s schools have been open since mid-April!! And, for those keeping score, Reuters just reported yesterday that, “Reopening schools in Denmark did not worsen outbreak, data shows.” Here’s a quote:
“You cannot see any negative effects from the reopening of schools,” Peter Andersen, doctor of infectious disease epidemiology and prevention at the Danish Serum Institute said on Thursday told Reuters. In Finland, a top official announced similar findings on Wednesday, saying nothing so far suggested the coronavirus had spread faster since schools reopened in mid-May.
Another great article on schools, titled, “It is fear – not science – that is stopping our children being educated” in The Telegraph newspaper last week, here’s a quote:
There is little about coronavirus we can be absolutely sure of – this is a brand new disease and our knowledge grows by the day – but most of the available evidence so far strongly suggests that children are neither suffering from coronavirus nor spreading it. Studies in South Korea, Iceland, Italy, Japan, France, China, the Netherlands and Australia all concur that youngsters are “not implicated significantly in transmitting Covid”, not even to parents and siblings.
Adult paranoia, stoked by over-the-top government messaging, union intransigence and media conniptions, is now being inflicted on the youngest members of our society to whom the virus poses a threat so tiny scientists call it “statistically irrelevant”. Instead of nursery rhymes, mixed infants may soon be invited to sing something called the “two-metre-song” as they stick their arms out to keep their friends at bay.
Brand new science (May 28) released from Northern Ireland clearly shows that schoolchildren do NOT serve as vectors for COVID-19. Titled, No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020, the study could not be more clear:
These findings suggest that schools are not a high risk setting for transmission of COVID-19 between pupils or between staff and pupils. Given the burden of closure outlined by Bayhem [4] and Van Lanker [5], reopening of schools should be considered as an early rather than a late measure in the lifting of restriction.
Finally, Dr. Scott Atlas took on the topic of schools in this recent interview:
“There’s no science whatsoever to keep K-through-12 schools closed, nor to have masks or social distancing on children, nor to keep summer programs closed. What we know now is that the risk of death and the risk of even a serious illness is nearly zero in people under 18.
Quick update: after I wrote this, the Wall Street Journal published this article titled Is It Safe to Reopen Schools? These Countries Say Yes. To me, this reads as a bit of a litmus test for countries that have independent and data-driven public health officials, and I give the U.S. an ‘F” for our current approach:
But Denmark, Austria, Norway, Finland, Singapore, Australia, New Zealand and most other countries that have reopened classrooms haven’t had outbreaks in schools or day-care centers…In Denmark, the opening of schools had no impact on the progress of the epidemic, said Tyra Grove Krause, a senior official with the State Serum Institute, the country’s disease control agency…Since Austria reopened on May 18, no increase in infections has been observed in schools and kindergartens, a spokesman for the government said…In Norway, the government won’t close schools again even if the number of cases starts rising in the country because there have been no negative consequences from reopening schools on April 20, said Education Minister Guri Melby.
How many more countries need to re-open before the U.S. follows? Seriously, it’s a little embarrassing to be American…IMO we look like total chumps.
Update #2: Dr. Scott Atlas doubled-down on June 1st with this great Op-Ed, once again in The Hill, titled Science says: ‘Open the schools’. As usual, he’s amazingly eloquent, here’s an excerpt but well worth the time to read every word, he simply slays it:
All of this borders on the absurd, when we now know that social distancing and face coverings for children are completely unnecessary.
Never have schools subjected children to such an unhealthy, uncomfortable and anti-educational environment, so science cannot precisely define the total harm it will cause. But science does tell us that risks from COVID-19 are too minimal to sacrifice the educational, social, emotional and physical well-being – to say nothing of the very health – of our young people.
(Special note: there’s a new boogeyman, Kawasaki disease, that some are trying to link to COVID-19. Here’s a great article about that, or see the website of the UK’s Kawasaki Disease Foundation where they discuss the “mishandling of information” about Kawasaki disease. Dr. Atlas’ most recent post discusses this, too: “What about the new threat similar to Kawasaki disease, recently sensationalized as a COVID-19 association? In fact, the association is extremely low, and the incidence of the disorder is itself rare, affecting only 3,000 to 5,000 children in the United States each year. Importantly, the syndrome is typically treatable and never has been regarded previously as a risk so serious that schools must be shuttered.”)
Fact #3: People infected with COVID-19 who are asymptomatic (which is most people) do NOT spread COVID-19

On January 13, 2020, a 22-year old female with a history of congenital heart disease went to the emergency room of Guangdong Provincial People’s Hospital complaining of a variety of symptoms common to people with her condition, including pulmonary hypertension and shortness of breath due to atrial septal defect (hole in the heart). Little did she know her case would set off a cascade of events resulting in a recently published paper that should have ended all lockdowns around the world simultaneously. Three days into her hospital stay, her condition was improving. Routine tests were run, and to the clinicians alarm and surprise, she tested positive for COVID-19. As the physicians noted, “the patient had never fever, sore throat, myalgia or other symptoms associated with virus infection.” Said differently, she was completely asymptomatic for COVID-19.
It’s not that easy to find people who are infected with COVID-19 but asymptomatic, because they don’t seek medical attention. Here in Oregon where I live, you can’t even get a COVID-19 test unless you have symptoms. So, the stars aligned to put this woman in a hospital with researchers studying COVID-19, and she became the subject of an extensive contact study published on May 13 in Respiratory Medicine, titled, “A study on infectivity of asymptomatic SARS-CoV-2 carriers.”
The researchers wanted to find out whether this woman, with a COVID-19 infection but no symptoms, had infected anyone else, so they chose to look at every single contact they could identify within the previous 5 days prior to her positive test. So, how many people did they have to screen? 455. Not a small number, as the researchers explain:
455 contacts who were exposed to the asymptomatic COVID-19 virus carrier became the subjects of our research. They were divided into three groups: 35 patients, 196 family members and 224 hospital staffs. We extracted their epidemiological information, clinical records, auxiliary examination results and therapeutic schedules.
As you can see, being hospitalized led to the majority of the contacts this woman had, both with other patients and with many members of the hospital staff. Notably, all of these contacts took place indoors and one might argue many of the contacts—at least with hospital staff—would have involved relatively intimate contact. Amongst the patients, the average age was 62, arguably making them higher risk, and many of those patients were immunocompromised for a variety of reasons, including chemotherapy and cardiovascular disease. So how many of the 455 people were infected by the asymptomatic 22-year old woman?
“In summary, all the 455 contacts were excluded from SARS-CoV-2 infection…”
Said differently, exactly zero people were infected. The scientists, in typically understated fashion, offer up a comment about the question I hope you are asking yourself right now (namely, why are we all on lockdown if asymptomatic people with COVID-19 can’t spread the infection?), stating, “the result of this study may alleviate parts of the public concern about asymptomatic infected people.”
If this study had been published in early March, the odds that the world would have locked down are very, very low. Yet, this study, published only two weeks ago, is nowhere to be found in the media, and is never mentioned by policy makers. It just sits there, sharing the truth for anyone willing to listen.
Fact #4: Emerging science shows no spread of COVID-19 in the community (shopping, restaurants, barbers, etc.)
“There is no significant risk of catching the disease when you go shopping. Severe outbreaks of the infection were always a result of people being closer together over a longer period of time…”
– Professor Hendrick Streek , University of Bonn
We just learned that asymptomatic people infected with COVID-19 are very unlikely to be able to spread the infection to others. Emerging and published science shows transmission of COVID-19 in retail establishments is extremely unlikely. Professor Hendrik Streeck from the University of Bonn is leading a study in Germany on the hard-hit region of Heinsberg and his conclusions, from laboratory work already completed, is very clear:

“There is no significant risk of catching the disease when you go shopping. Severe outbreaks of the infection were always a result of people being closer together over a longer period of time.
“When we took samples from door handles, phones or toilets it has not been possible to cultivate the virus in the laboratory on the basis of these swabs….”
Uh oh. You mean closing parks, closing stores, wearing gloves and masks at the grocery store, fumigating our groceries, and just being generally paranoid wasn’t necessary? As Dr. Streeck confirms:
“It is important to obtain this data in order to make sure that decisions are taken based on facts rather than assumptions. The data should serve as a basis of information for the government so they can then think about their further course of action,” he said.
And he continues:
“People could lose their jobs. They might not be able to pay their rent anymore and staying inside for a longer time can lead to weakening of our immune system.”
“The goal is not a complete containment of the virus. We need to know where the actual capacity limits of our hospitals are. How many infections are too many? What do intensive care medics say?”
And, finally:
“It is important to start thinking about a ‘rollback’ strategy and his hope is to “deliver the relevant facts so that people have a good foundation for their decisions.”
Fact #5: Published science shows COVID-19 is NOT spread outdoors

In a study titled Indoor transmission of SARS-CoV-2 and published on April 2, 2020, scientists studied outbreaks of 3 or more people in 320 separate towns in China over a five-week period beginning in January 2020 trying to determine WHERE outbreaks started: in the home, workplace, outside, etc.? What’d they discover? Almost 80% of outbreaks happened in the home environment. The rest happened in crowded buses and trains. But what about outdoors? The scientists wrote:
“All identified outbreaks of three or more cases occurred in an indoor environment, which confirms that sharing indoor space is a major SARS-CoV-2 infection risk.”
Said differently, there’s really no science to support all the outdoor bans that my home state of Oregon and so many other states have put in place. I’ll leave you with my favorite quote from the study because it’s really quite infuriating to read when you consider some of the ways Governors here in the U.S have behaved (and some still do) by banning all sorts of outdoor activities, arresting paddle boarders on the water, etc.:
“The transmission of respiratory infections such as SARS-CoV-2 from the infected to the susceptible is an indoor phenomenon.”
Quick Update: Apparently the health minister of British Columbia, Canada, got the memo about the lack of airborne risk, this article appeared on June 1:

One of B.C.’s top health officials, however, says medical professionals have a pretty clear picture of how the virus is transmitted. “There is absolutely no evidence that this disease is airborne, and we know that if it were airborne, then the measures that we took to control COVID-19 would not have worked,” Dr. Reka Gustafson, B.C.’s deputy provincial health officer, told CTV Morning Live Monday.”We are very confident that the majority of transmission of this virus is through the droplet and contact route….”The overwhelming majority of (COVID-19) transmissions occur through close, prolonged contact and that is not the pattern of transmission we see through airborne diseases,” she said.
I sure hope Major League Baseball, the National Football League, and the NCAA are all paying attention…not to mention all the people in Portland here still riding bikes and running with masks on.
Fact #6: Science shows masks are ineffective to halt the spread of COVID-19, and The WHO recommends they should only be worn by healthy people if treating or living with someone with a COVID-19 infection
May 29th, the World Health Organization announced that masks should only be worn by healthy people if they are taking care of someone infected with COVID-19:
“If you do not have any respiratory symptoms such as fever, cough or runny nose, you do not need to wear a mask,” Dr. April Baller, a public health specialist for the WHO, says in a video on the world health body’s website posted in March. “Masks should only be used by healthcare workers, caretakers or by people who are sick with symptoms of fever and cough.”
Just before the COVID-19 madness, researchers in Hong Kong submitted a study for publication with the mouthful of a title, “Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures.” Oddly, the study, just published this month, is actually housed on the CDC’s own website, and directly contradicts recent advice from the CDC about wearing a mask. Namely, the study states:
“In our systematic review, we identified 10 RCTs that reported estimates of the effectiveness of face masks in reducing laboratory-confirmed influenza virus infections in the community from literature published during 1946–July 27, 2018….In pooled analysis, we found no significant reduction in influenza transmission with the use of face masks…Our systematic review found no significant effect of face masks on transmission of laboratory-confirmed influenza….Proper use of face masks is essential because improper use might increase the risk for transmission.”
English translation: there is no evidence that wearing masks reduces the transmission of respiratory illnesses and, if masks are worn improperly (like when people re-use cloth masks), transmission could actually INCREASE. Moreover, this study was a meta-analysis, which means it dug deep into the archive of science (all the way back to 1946!) to reach its conclusions. Said differently, this is as comprehensive as science gets, and their conclusions were crystal clear: masks for the general population show no evidence of working to either slow the spread of respiratory viruses or protect people.
This study is far from the only one to reach this conclusion (which makes the choice of a grocery store chain like my beloved New Seasons to make masks mandatory for all customers really quite unbelievable). The purpose of science is to arbitrate these thorny issues and while the science is clear, the hysteria continues. It turns out, the effectiveness of masks has a long history of debate in the medical community, which explains why so much science has been done on the topic. I will just highlight a few studies before you fall asleep:
My favorite article is actually a review of much of the science and it’s a great place to start for anyone who likes to do their own research. Titled, “Why Face Masks Don’t Work: A Revealing Review”, it was written to challenge the need for dentists to wear face masks, but all the science quoted and conclusions drawn apply to airborne pathogens in any setting. Some of the best quotes:
“The science regarding the aerosol transmission of infectious diseases has, for years, been based on what is now appreciated to be ‘very outmoded research and an overly simplistic interpretation of the data.’ Modern studies are employing sensitive instruments and interpretative techniques to better understand the size and distribution of potentially infectious aerosol particles…The primary reason for mandating the wearing of face masks is to protect dental personnel from airborne pathogens. This review has established that face masks are incapable of providing such a level of protection.”
And my favorite quote:
“It should be concluded from these and similar studies that the filter material of face masks does not retain or filter out viruses or other submicron particles. When this understanding is combined with the poor fit of masks, it is readily appreciated that neither the filter performance nor the facial fit characteristics of face masks qualify them as being devices which protect against respiratory infections. ”
Here’s an article published in ResearchGate by noted Canadian physicist D.G. Rancourt, written directly in response to the COVID-19 outbreak, published last month. Titled, Masks Don’t Work: A review of science relevant to COVID-19 social policy.
“Masks and respirators do not work. There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles. Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective-dose is smaller than one aerosol particle.”
To put this in simple terms: in order for a mask to really be effective that covered both your nose and mouth, you would asphyxiate. The minute the mask allows you to breathe, it can no longer filter the micro-particles that make you sick.
Finally, I often see this study from 2015 in the BMJ cited: “A cluster randomised trial of cloth masks compared with medical masks in healthcare workers“, and it bears repeating, since MOST of the masks I see people wearing in the community right now are cloth masks. Not only are these masks 100% ineffective at reducing the spread of COVID-19, but they can actually harm you. As the researchers explain:
“This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Further research is needed to inform the widespread use of cloth masks globally.”
Increased risk of infection? Yes, that’s what it says. Other studies have also looked at the impact masks have on your oxygen levels (because you’re are forced to re-breathe your own Co2) and it’s not good. Scientists looked at oxygen levels of surgeons wearing masks while performing surgery and found: “Our study revealed a decrease in the oxygen saturation of arterial pulsations (SpO2) and a slight increase in pulse rates compared to preoperative values in all surgeon groups.”
Just this past week, this article came out in the New England Journal of Medicine, written my several doctors and public health officials with the title, “Universal Masking in Hospitals in the Covid-19 Era,” and this statement seems a perfect way to end my discussion of masks:
We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.
Read the rest here: https://childrenshealthdefense.org/news/lockdown-lunacy-the-thinking-persons-guide/